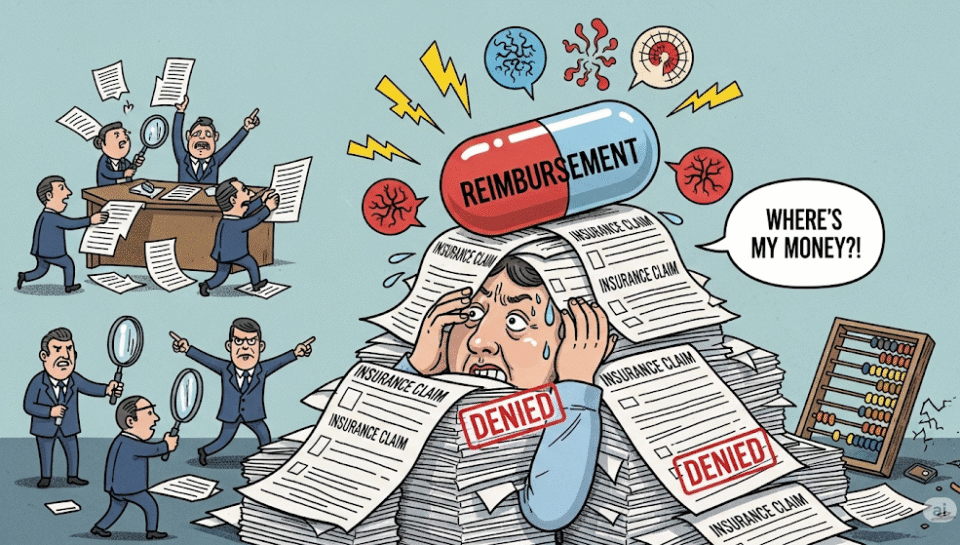
If you feel like you need an adjustment every time you check your accounts receivable, you may be suffering from a classic case of “insurance reimbursement frustration.” Late, denied, or partial payments from insurers keep many chiropractic practices up at night—and the ripple effects can be brutal for your business.
Why Claims Aren’t Getting Paid
- Coding errors: Even a single typo can result in rejection.
- Missing documentation: Incomplete notes or forms mean insurers have an “easy out.”
- Late filing: Many insurers have tight deadlines; wait too long and your claim is toast.
- Eligibility changes: Patient switched coverage? You might be the last to know.
How These Reimbursement Delays Hurt Chiropractors
- Cash flow takes a hit, making it hard to cover payroll or supplies.
- Admin staff spends hours chasing down payments instead of helping patients.
- Your stress spikes—you start dreaming in ICD-10 codes (which honestly, nobody wants).
Solutions for Timely Reimbursement
1. Tighten Documentation:
Chart in real time, keep thorough notes, and double-check forms before submission.
2. Get Coding Help:
Don’t DIY—use billing software built for chiropractic, or work with a pro who lives by the code books.
3. Follow Up Like a Pro:
Don’t let claims languish. Create a follow-up calendar and don’t be shy about contacting insurers.
4. Automate Claims Where Possible:
Cloud-based systems track, flag, and resubmit claims automatically—much better than sticky notes.
Final Thought
Smooth reimbursement flow means more time on patient care, less time fighting paperwork, and (best of all) fewer insurance-induced headaches. Ready for real relief? SkillBench helps chiropractors get paid—so you can focus on healing, not chasing claims.